Background: SARS-CoV-2 infection has been associated with profound infection-induced inflammatory changes including coagulopathy (Connors et al. Blood 2020). Furthermore, venous thromboembolism (VTE) has been described as a common complication among patients with COVID-19 (Tang et al. J Thromb Haemost 2020). Patients with a history of HM who contract SARS-CoV-2 may be at an even higher risk for VTE, given their elevated baseline VTE risk; however, there is limited clinical data for this patient population. Therefore, we performed a retrospective chart review to evaluate clinical outcomes in patients with COVID-19 and a history of HM.
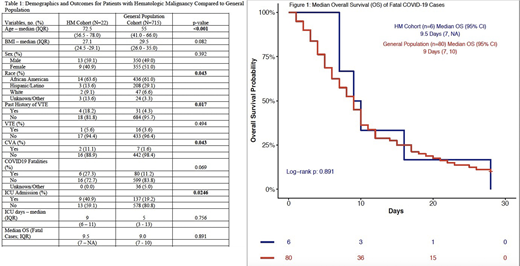
Methods: A REDCap database was created using all patients who were evaluated in the emergency department or admitted to MedStar Georgetown University Hospital/Washington Hospital Center with a confirmed SARS-CoV-2 diagnostic test between March and May 2020. Data extraction was performed on all patients to identify demographic and clinical parameters. All data collected reflects clinical encounters related to COVID-19 infection. Our primary end-point was rate of VTE and cerebrovascular accident (CVA) in patients with HM compared to the general population. Secondary outcomes assessed were COVID-19 related mortality, Intensive Care Unit (ICU) admission rates, and length of ICU stay. Continuous variables were summarized by median quartiles (Q1 and Q3) and categorical variables were summarized by frequency counts and percentages for each category. The two-sample t-test for continuous variables and binomial exact test or Pearson chi square test for categorical variables were conducted to compare the means/distributions of each variable between HM patients and the general population, respectively. The Kaplan-Meier method and log-rank test were used to evaluate and compare the median overall survival (OS) between the two groups, exclusively for patients who died from COVID-19, censored at 28 days from admission.
Results: As of July 1st, 2020, 737 pts with COVID-19 have been identified and included in this preliminary analysis. Twenty-two pts had a HM: plasma cell dyscrasia (n=7, 31.8%; multiple myeloma n=6, MGUS n=1), chronic lymphocytic leukemia (n=3, 13.6%), chronic myelomonocytic leukemia (n=2, 9.1%), diffuse large B-cell lymphoma (n=2, 9.1%), hodgkin's lymphoma (n=2, 9.1%), and one patient (4.5%) with each of the following malignancies: acute promyelocytic leukemia, anaplastic large cell lymphoma, B-cell lymphoma not otherwise specified, follicular lymphoma, mantle cell lymphoma and marginal zone lymphoma. With respect to HM treatment status, the majority of the patients were in surveillance (n=14, 63.6%); the other eight (36.4%) were on active treatment at time of COVID-19 infection. In patients who had a remission status documented, eight showed complete remission (36.4%), five with partial remission (22.7%), and one patient with progressive disease (4.5%). Six patients (27.3%) either did not yet have a remission status evaluated or were treatment naïve. The HM cohort was found to be older (median age 72 vs. 55) and have a higher rate of historical VTE prior to COVID-19 infection (18.2% vs. 4.3%). Other demographic data for the HM cohort and the general population can be found in Table 1. CVA was more prevalent in the HM cohort compared to our general population cohort (11.1% vs. 1.6%, p = 0.048). Rates of VTE were not statistically different between the two groups (5.6% vs. 3.6%, p=0.494). A higher percentage of HM pts required ICU admission (40.9% vs. 19.2%, p = 0.0246). Our data suggested a trend towards higher rate of case fatality in the HM cohort (27.3% vs. 11.2%, p = 0.069) and a trend towards longer duration of ICU admission (9 days vs. 5 days, p=0.756). The median OS in fatal COVID-19 infection (Figure 1) was 9.5 days (95% CI, 7 to NA) in the HM cohort compared to 9 days (95% CI, 7 to 10, p=0.891) for the general population.
Conclusion: Our preliminary findings suggest among patients with COVID-19, there is an increased incidence of CVA in HM patients, but similar rates of VTE when compared to the general population. Our HM cohort had higher rates of ICU admission, but did not have a statistically significant mortality difference at 28 days. Data collection is ongoing, final analysis will be completed with a larger cohort of HM patients.
Lai:Abbvie: Consultancy; Agios: Consultancy; Macrogenics: Consultancy; Astellas: Speakers Bureau; Jazz: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.